Sedation in Dentistry Nervous Patients Many people are a bit anxious about attending a dentist. For some people however, this fear is more pronounced and can be classified as a dental phobia.…
Orthodontic treatment
Swords Dental are delighted to announce that we will now be providing a full range of orthodontic treatment for our patients. Our Orthodontist, Dr. Greice Zanotti, from Brazil offers fixed and removable…
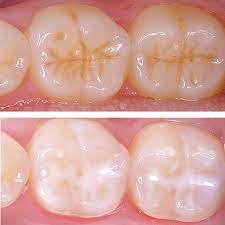
Fissure Sealants
Fissure Sealants The adult first permanent molar teeth tend to come into the mouth at just six years old. This is a critical period for fissure sealants because the diet between 6-12…
VHI Dental Insurance
VHI Dental Insurance Swords Dental is a member of the Vhi Direct Pay Dental Network. Vhi Dental members can avail of Direct Payment of their plan benefits when they attend a dentist…
Implants
Implants Durable, long-lasting and natural in their appearance, dental implants are the most modern method of replacing missing teeth. The procedure involves fitting an implant which is usually made of titanium, into…
Swords Dental
This new website at Swords Dental gives us an opportunity to explain the ethos of our practice. Swords Dental is the longest-established dental practice based in Swords, Co Dublin. We are a…
Invisalign™ at Swords Dental
Invisalign™ at Swords Dental Swords Dental are thrilled to announce that we will now offering Invisalign to our patients. We will be hosting an Invisalign open day on Sat 1st May. We…
Dental Cleaning
Dental Cleaning for PRSI Patients Patients who are covered by PRSI ( including the self-employed) are now entitled to a free check up and subsidised dental cleaning at a cost of 15…
Composite Bonding
Composite Bonding The demand for cosmetic dentistry is increasing, with whitening procedures, braces and veneers becoming more and more common. The problem is, braces can be a slow and painful process, and veneers involve…
Facial Aesthetics
Facial Aesthetics Facial aesthetics are a range of non-surgical treatments that are now available at Swords Dental Facial aesthetics soften expression lines on a temporary basis. With in-depth anatomical knowledge of the face…